Courtney Scales DipVN, NCert(Anaesth), RVN
Keith Simpson BVSc, MRCVS, MIET(Electronics) – Clinical Director
Joel Huey BA (Hons) – Content Editor
Total Read Time: 20 minutes
The decision to buy a new veterinary ventilator for the practice is not one that should be taken lightly. Aside from the capital investment, some things should be considered during the decision process, including the needs of the patient, whether the staff using the ventilator understand the concepts of ventilation and are confident in performing them and then finally, what type of ventilator suits the practice.
This blog discusses why a patient may require support with their ventilation and then explores the issues above, before setting out a framework to follow that ensures your practice is ready to receive and work with a new ventilator.
Respiratory-related Anatomy and Physiology
The main function of the respiratory system is to facilitate gas exchange during inhalation and exhalation. Oxygen is inspired and then diffuses into the blood for use in the tissue, and then carbon dioxide (CO2), a waste product of cellular metabolism, is exhaled.
Ventilation is either performed by the patient spontaneously breathing or through assisted breathing by the anaesthetist:
• During spontaneous breathing, a sub-atmospheric pressure is created in the pleural space when the intercostal muscles and diaphragm contract, “pulling” air into the lungs.
• Conversely, Intermittent Positive Pressure Ventilation (IPPV) is when air is forced or “pushed” into the lungs manually (by squeezing the reservoir bag) or mechanically (using a ventilator).
When does a patient require IPPV?
A patient may require IPPV for several reasons depending on their clinical situation, disease process or the procedure being performed. There are three main reasons supportive ventilation may need to be provided:
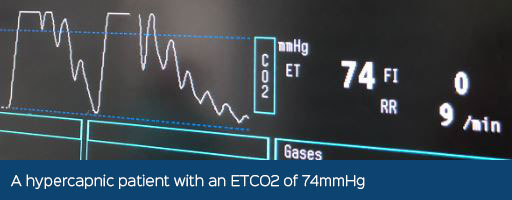
1. The patient cannot ventilate adequately (PaCO2 or ETCO2 >60mmHg), for example:
• Most anaesthesia drugs cause dose-dependent depressive effects on the central nervous system, where the respiratory centre is
• Patients with specific body conformations, such as obesity, will have a reduced Functional Residual Capacity (FRC) as there is weight pushing on the diaphragm, reducing the volume of lung available for gas exchange in between breaths.
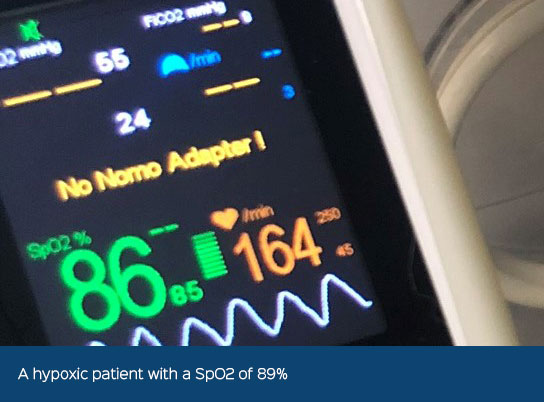
2. The patient cannot oxygenate (PaO2 <60mmHg or SpO2 <90%), but consider:
• Hypoxaemia is less common in intubated patients with healthy lungs that are under anaesthesia and receiving high inspired oxygen concentrations, compared to patients in which the lungs are already diseased, where there may not be an improvement in oxygenation.
• There is nitrogen in room air which does not diffuse across the alveoli and instead can “hold” them open. Under anaesthesia, when breathing high concentrations of oxygen which diffuse readily from the alveoli, there is no nitrogen to hold the alveoli open, which can lead to alveolar collapse or atelectasis, causing a Ventilation/Perfusion (V/Q) mismatch.
3. If there is impaired respiratory muscle function, then the usual physiology in how the lungs draw in air is lost. This may occur in patients with:
a. A diaphragmatic hernia or thoracic wall injury.
b. The phrenic nerve, which innovates the diaphragm, exits between the 4th and 7th cervical vertebrae and may become damaged in patients with high spinal fractures or those with cervical spinal cord compression.
c. When using neuromuscular blocking agents (NMBAs) that paralyse skeletal muscle.
Other reasons a patient may require IPPV are those that have induction apnoea, have excessive anaesthesia depth, are hypothermic, have raised intracranial pressure or in patients with myasthenia gravis.
The difference in providing IPPV for patients under anaesthesia versus critical care is that patients under anaesthesia are receiving high concentrations of oxygen already, so hypoxaemia is not usually an issue. Therefore, ventilation during anaesthesia is most often performed due to hypercapnia and is short-term in comparison to patients being ventilated in an intensive care setting. These often have lung pathology and usually require ventilation for hypoxia or due to the inability to adequately oxygenate.
Positive Effects of IPPV
Being aware of the possible side effects of IPPV is crucial in being able to deliver safe automatic ventilation. However, generally the positive benefits outweigh the negative.
The positive effects of IPPV include:
- • Controlled delivery of oxygen to the patient. Providing consistent deep breaths ensures an adequate volume of oxygen is delivered to the lungs
- • Controlled removal of CO2 from the patient. Maintaining a minimum minute volume ventilation ensures adequate exhalation of CO2.
- • Controlled delivery and/or removal of inhalation agent. By controlling ventilation minute volume the consistent delivery or removal of volatile anaesthetic agent is assured.
- • Markedly reduces the work of breathing for the patient. Weak, elderly or otherwise compromised animals will benefit from the assistance provided by mechanical IPPV
- • Greater control of depth of, and recovery from, anaesthesia
- • The ability to rapidly respond to changes in CO2 levels and minimise induced acid-base disturbances.
Negative effects of IPPV
There are negative and potentially harmful effects when providing IPPV which must be managed carefully through patient monitoring and with the understanding of safe ventilation techniques. These effects include:
- • A reduction in cardiac output that may occur due to the physiological thoracic pump being affected, a reduction in venous return or even cardiac tamponade (by the overinflated lungs).
- • There may be negative cerebral, coronary, renal and hepatic effects due to the changes in blood pressure which can compromise blood flow to these organs.
- • Damage to the lung can occur due to alveolar rupture or with the release of inflammatory mediators.
- • Blood gas and acid-base disturbances may occur, even if you are unable to monitor this directly with blood sampling.
Manual or Mechanical IPPV?
There are many benefits to using a ventilator instead of performing manual IPPV, including:
- • The ability to provide consistent delivery of anaesthesia gases, reducing fluctuations in anaesthesia depth.
- • Manual IPPV is not sustainable in the long term due to a dedicated staff member always being required.
- • Hypercapnia may occur if breaths cannot be delivered for some time.
During manual IPPV, the patient is at risk of iatrogenic injury. For example, with unknown pressures and volume delivered to the lungs or by accidentally leaving the APL valve closed.
As you can appreciate, a ventilator ensures safe volumes and pressures are delivered to the patient at an appropriate rate and they have many alarms and safety features built into them, reducing human error.
Considerations when buying a ventilator
A veterinary practice may look to purchase a ventilator for several reasons. It may be that the practice has started doing more advanced procedures, such as thoracotomies or ophthalmic procedures using NMBAs, which necessitate a ventilator, or it may that the general increase in surgery caseloads means that much more manual IPPV is being performed than before.
Whatever the reason, there are some questions that immediately arise surrounding the purchase, which includes:
- 1. Who within the practice has the training and skills to confidently use the ventilator?
- 2. Can you identify someone in the practice who will take charge and be responsible for the care and maintenance of the ventilator daily?
- 3. Are all staff to be trained on the use of the ventilator or just a select few?
- 4. Where will that training come from?
- 5. Will the ventilator be available for use on all patients or just on a select few?
- 6. What species range will the ventilator be used on?
- 7. Will any additional equipment be needed to support the use of a ventilator?
- 8. Will the current gas supplies be sufficient to support the new ventilator?
- 9. Where will the ventilator be used?
- 10. Is there space for a ventilator?
Whatever the reasons for the need to purchase a new ventilator, the first 4 points above are the most important things to consider:
- • They will be dependent on the existing skill set of the team in the practice. Learning the skills for ventilation takes time and is not something that can, or should, be learned as you go. If possible, seek training or gain CPD experience on ventilation before deciding what ventilator to purchase. This may include visiting a practice that is routinely using ventilators to see how they approach the whole subject of routine patient ventilation, attending webinars or watching videos online that show how to use the ventilator you are looking to purchase.
- • Taking the first of the ten points above, do you already have someone in the practice that has been trained to use a ventilator for the purposes that are expected? Is that person confident to take on the role of ventilator ‘trainer’ or could they benefit from some more training?
There are certain skills and knowledge levels required from someone considering ventilating a patient under anaesthesia, including the understanding of:
- 1. The need for endotracheal intubation and why the trachea should be “sealed”.
- 2. The physiology and control of breathing and its application to the anaesthetised patient.
- 3. The role of CO2 in patient homeostasis and its effect on the patient.
- 4. The mechanics of manual IPPV and its influences compared to spontaneous breathing.
- 5. The different modes of ventilation and when to apply them.
- 6. The concept of minute volume and its variation over time, depending on clinical and monitor feedback.
- 7. The need for minimised dead space and how to minimise the effect of dead space.
- 8. The concept of compliance and its influence on the ventilated patient.
After understanding and considering the needs of the patient, it is important to consider the specific set-up and preparation of a particular ventilator, based on the knowledge of:
- 1. The breathing system configurations and types commonly used with ventilators.
- 2. Integration of the ventilator with common circle systems and/or the Humphrey ADE system.
- 3. What will drive the ventilator - pressurised oxygen, pressurised air, both, or none?
- 4. How are waste gases from the ventilator scavenged?
- 5. Is there a procedure to follow in case of power loss to the ventilator?
The two lists of points above are general requirements when considering ventilation and should be taken as the minimum level of understanding needed before ventilating a patient during anaesthesia.
Getting Started
If there is no one in the practice that has been trained on the use of ventilators, then we highly recommend someone obtains training before starting to use the new ventilator. It would be inappropriate to use or demonstrate the use of a ventilator in practice before its purchase without understanding the fundamentals first.
This type of training suggested covers several disciplines:
- • Ventilation
- • Breathing Systems
- • Capnography
- • Dead Space
All four of these areas are involved in the ventilation of a patient, and they are all interdependent. For example, it is difficult to understand the workings of breathing systems without understanding dead space and fresh gas flow. And it is difficult to understand the impact of dead space without understanding what capnography represents.
This is our suggested framework to follow when buying a new ventilator:
- 1. Identify the ventilator type most suited to your patients and your practice. (It is important to note that some ventilators are used in human medicine which may not be suitable for some veterinary patients that are <10kg due to the inability to provide small tidal volumes).
- 2. Determine where the ventilator will be sited and how it will be integrated into the operating room.
- 3. Identify personnel in the practice that are already sufficiently skilled to use the ventilator OR
- 4. Identify personnel in the practice that are willing to undergo training on ventilation.
- 5. Select a provider to deliver any ventilation training you require.
- 6. Set aside some time to learn how to use the new ventilator, preferably by using it with a simulation patient (e.g. the Annequin)
- 7. Train all staff in the setup, cleaning and checking of the ventilator.
- 8. Determine if you need any extra equipment to support the ventilator, e.g. capnograph, blood pressure monitor or new endotracheal tubes
Conclusion
Whilst this blog has not set out to suggest a particular ventilator, we do have a range of ventilators covering a whole species range from mice to horses! If you require any help or advice in identifying the best ventilator suited to your practice, please contact us.
In addition to a range of ventilators, we have advanced patient simulation aids to help you learn more about ventilation before using it on a live patient and we can provide ventilator training and support if required.
Burtons Veterinary Equipment YouTube Videos
The Vetronic Merlin Ventilator - An In-Depth Guide
Introduction to the Vetronic SAV04 Ventilator
Introduction to The Annequin Training Model - Part 1/4
Want to Learn more about ventilation? You can browse our CPD courses here
Burtons Veterinary Equipment Products
Ventilators
If you are looking for one ventilator for all of your small animal practice needs, from small rodents to large dogs, then the Vetronic Merlin Ventilator is your ideal solution. Designed for Vets, by Vets, the Merlin uses the latest technology to precisely control ventilation parameters, ensuring your patient is as safe as can be during mechanical ventilation, and, because it is controlled by a state-of-the-art microcontroller, you can confidently set the independent ventilation parameters that you want, without compromise.
If you are needing to ventilate patients 12kg and under, then the compact Vetronic SAV04 Ventlator is for you. A safe, simple way to ventilate your smaller, most vulnerable patients, the SAV04 incorporates a host of features for improved control of IPPV. These include an automatic over-pressure alarm that will sound if the target pressure is exceeded by 8cm and a screen that displays a central rising bar graph showing the pressure in the patients airway, as well as the inspiratory period measurement.
Training models
The Annequin (animal mannequin) is a dummy animal capable of accurately emulating the behaviour and responses seen in ventilated animals with respect to CO2 elimination. It can be used with any standard ventilator and any form of capnograph. It mimics a normal animal by having a constant rate of CO2 production that must be removed by ventilation. This allows safe practical training for vets and nurses in responses to emergencies in ventilation.



